The human immune system is a complex network designed to protect the body from harmful pathogens such as bacteria, viruses, and parasites, as well as to repair damage caused by injuries. While its role in pathogen defense is well-understood, recent research has revealed that immune cells are also crucial in tissue repair and the resolution of inflammation. This dual role becomes especially significant in the context of chronic inflammatory diseases, where the immune system either becomes dysregulated or overreacts, leading to tissue damage and disease progression.
Chronic inflammation occurs when the immune system fails to properly regulate its response, causing prolonged tissue damage and exacerbating various health conditions. A deeper understanding of how the immune system communicates within itself and with other cells of the body is essential for unraveling the complexities of these diseases. Endometriosis, for example, is one such disease where immune cells play a central role in both the disease’s onset and progression.
The Innate and Adaptive Immune System: A Coordinated Defense Mechanism
The immune system is typically divided into two key branches: the innate and the adaptive immune responses. The innate immune system is the first line of defense, quickly recognizing molecular patterns that indicate potential threats. These patterns, called pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs), signal the presence of harmful microorganisms or tissue injury. The adaptive immune system, on the other hand, provides a more specialized and tailored response to these threats, typically activating only after the innate system has failed to clear the threat effectively.
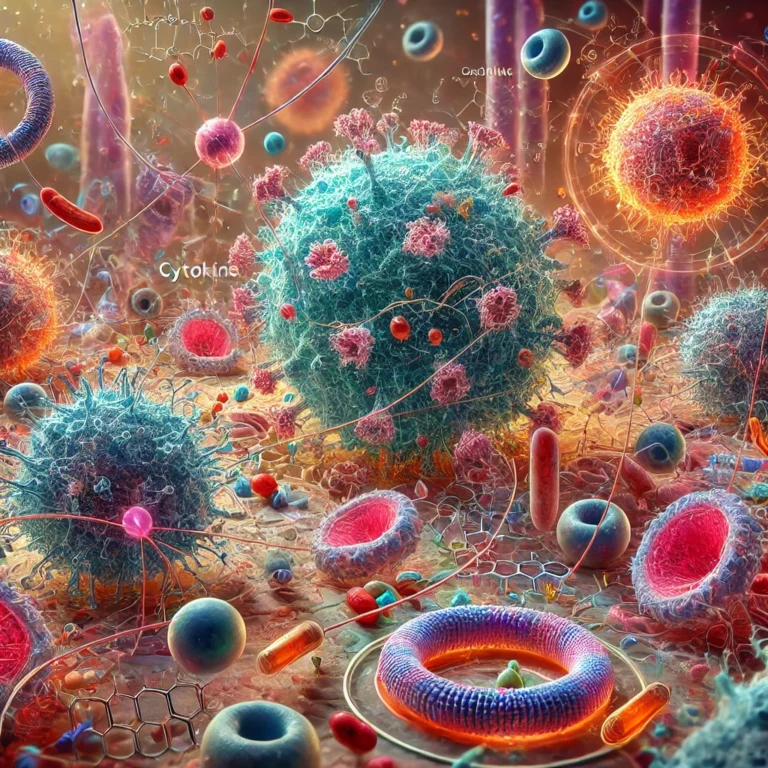
Recent research suggests that the interaction between the innate and adaptive immune systems is not a simple sequential process, but rather a dynamic and highly interconnected network. Cytokine signaling between these two branches helps fine-tune the immune response, ensuring that it is appropriate to the nature of the threat. Importantly, the communication between immune cells and non-immune tissue cells also plays a crucial role in deciding whether the immune system should activate an inflammatory response or dampen it to avoid excessive tissue damage.
Understanding these interactions is crucial for developing therapeutic strategies that can either enhance or suppress specific immune responses depending on the context. In conditions of chronic inflammation, where the immune system is overactive or improperly regulated, the result can be tissue destruction, as seen in diseases like autoimmune disorders and endometriosis.
Endometriosis: A Complex Dance Between Immune Cells and Tissue Damage
Endometriosis is a condition where tissue similar to the lining of the uterus, called endometrial tissue, grows outside of the uterus. This abnormal tissue growth leads to a variety of symptoms, including pelvic pain, infertility, and chronic inflammation. It affects approximately 6-10% of women of reproductive age and is a leading cause of infertility. While the exact cause remains elusive, researchers have long proposed that retrograde menstruation — where menstrual blood flows backward through the fallopian tubes into the pelvic cavity — could be a key factor in disease development. However, retrograde menstruation occurs in around 90% of women, and not all of them develop endometriosis, suggesting that other factors are at play, particularly immune system dysfunction.
The immune system plays a pivotal role in the pathogenesis of endometriosis. When endometrial tissue is shed and refluxes into the pelvic cavity, immune cells are called to the site of injury to clear the tissue and repair any damage. However, in women with endometriosis, this process goes awry. Rather than effectively eliminating the abnormal tissue, the immune system’s response exacerbates the problem, leading to the chronic inflammation that characterizes the disease.
Macrophages, a type of white blood cell, are particularly involved in this process. These cells are typically responsible for clearing dead or damaged cells through a process known as phagocytosis. However, in the case of endometriosis, macrophages are persistently activated by signals from the ectopic (abnormal) endometrial tissue. This leads to an inflammatory feedback loop, where macrophages release cytokines such as RANTES and IL-13, which promote further inflammation and angiogenesis — the formation of new blood vessels — essential for the survival and growth of endometriotic lesions.
The Role of Immune Dysregulation: Apoptosis, Necrosis, and Inflammation
In a healthy immune response, when tissue is injured, it undergoes a process of apoptosis, or programmed cell death, which prevents the release of harmful substances and limits inflammation. In endometriosis, however, apoptosis is impaired in both eutopic (normal) endometrial cells and the shed endometrial tissue. This failure to undergo apoptosis allows the refluxed tissue to survive and establish itself in the pelvic cavity. If these cells do not undergo apoptosis, they may experience necrosis — a form of cell death that triggers a more intense inflammatory response.
Necrotic cells release a variety of molecules known as damage-associated molecular patterns (DAMPs), such as high mobility group box 1 (HMGB1) and heat shock proteins, which further activate the immune system and promote a wound-healing response. This creates a vicious cycle, as the immune system’s efforts to repair tissue instead fuel the chronic inflammation characteristic of endometriosis.
Macrophages and Angiogenesis: The Critical Immune Cell in Endometriosis
Macrophages in women with endometriosis often exhibit a phenotype associated with alternative activation, which is crucial for wound healing and angiogenesis. These alternatively activated macrophages release growth factors that promote blood vessel formation, which in turn supports the survival and growth of endometriotic lesions. Studies have shown that macrophage activation is closely linked to increased lesion size and severity in animal models of endometriosis.
Furthermore, research has shown that cytokines secreted by macrophages in the peritoneal fluid of endometriosis patients can influence the behavior of endometrial stromal cells. These cells, both eutopic and ectopic, secrete RANTES, a chemokine that attracts more macrophages to the site of injury. This positive feedback loop accelerates the inflammatory environment, making it difficult for the body to resolve the damage and return to a state of immune homeostasis.
Therapeutic Implications: Targeting the Immune Response in Endometriosis
A better understanding of the immune system’s role in chronic inflammatory diseases like endometriosis offers exciting therapeutic possibilities. Targeting specific immune responses could help regulate inflammation, promote tissue repair, and prevent disease progression. For instance, therapies that modulate macrophage activation or inhibit the release of inflammatory cytokines could provide relief for women suffering from the debilitating symptoms of endometriosis. Additionally, understanding how immune cells interact with non-immune cells in the peritoneum could pave the way for more targeted and effective treatments that not only alleviate symptoms but also address the underlying causes of chronic inflammation.
Conclusion: The Interplay Between Immune Cells and Tissue in Chronic Inflammation
The immune system’s role in chronic inflammatory diseases like endometriosis highlights the complexity of immune regulation. Rather than simply responding to pathogens, immune cells like macrophages play an active role in both tissue repair and inflammation, influencing the outcome of diseases. The failure of the immune system to appropriately balance these responses can lead to chronic inflammation, tissue damage, and disease progression. By studying these processes more thoroughly, we can uncover new strategies for managing and potentially curing diseases driven by immune dysfunction.